Intended for Consumer Use
LiveO2 A/C and ACX Systems are in stock
The patented LiveO2 Adaptive Contrast (AC) System is our most popular system. This system allows you to train with all our exercise usage guides. Our proprietary Adaptive Contrast technology allows you to instantly switch between oxygen concentrated air and oxygen depleted air. This allows you to get better results in less time.
Who it is For
This system is a great fit for any home. It allows you to train using Adaptive Contrast technology in the comfort of your home. With this system you can complete all our exercise usage guides. Because a Standard EWOT system does not have Negative O2 (oxygen depleted air) you can only complete basic exercise usage guides.
We recommend professional athletes and institutions use our Dual AC System.
Design
Adaptive Contrast System takes up the same footprint as our Standard system. If you upgrade to the 20LPM option you will get two oxygen concentrators.
The AC system uses a more powerful concentrator technology so you can fill a system in as little as 20 minutes (20 LPM Option) or 1 hour (10 LPM Option).
Reservoir Size:
- Reservoir Height = 7 Feet
- Reservoir Width with stand = 5 Feet
- Reservoir Depth = 3 feet
- The reservoir will fit in any room with normal ceiling height
- Allow additional floor space for exercise equipment.
Adaptive Contrast Technology
Patented Adaptive Contrast (AC) technology gives you access to both oxygen concentrated air and oxygen depleted air. It is the newest generation of our exercise with oxygen technology.
By training with oxygen depleted air your cells quickly create an increased demand for oxygen. When you flip the switch back to higher oxygen air your cells can absorb more oxygen.
Benefits of using AC over Standard (EWOT) reservoir systems include:
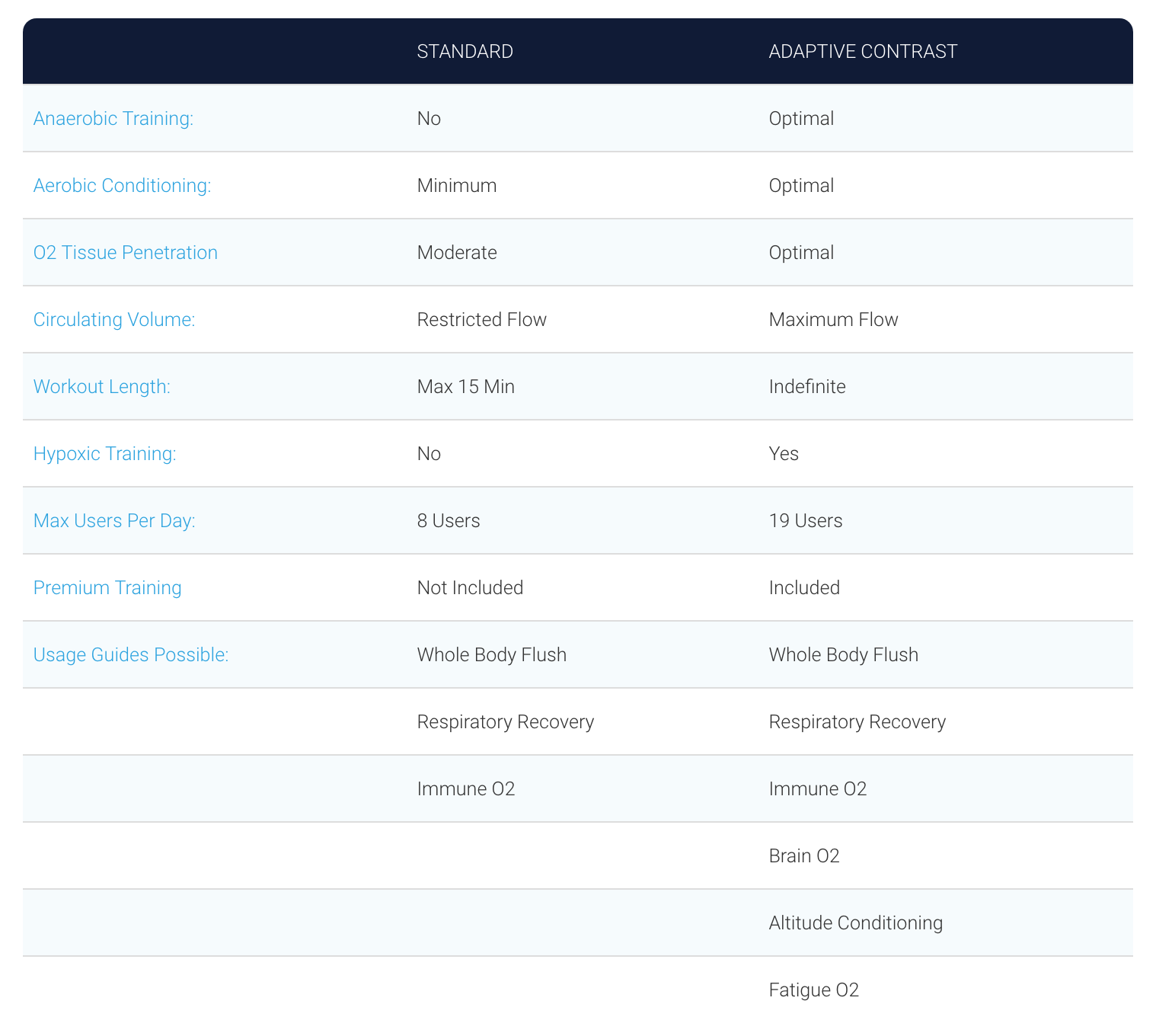
- Increased levels of oxygen in blood plasma and tissues
- Creating more red blood cells
- Expansion of vascular networks
- Greater energy and cellular voltage
- Faster recovery/healing/performance
- Having an AC system also allows you to use all the guides on our website.
Premium Support & Training
Included Premium Support for Adaptive Contrast:
- Phone or Video Support
- Unlimited Product Support
- Private LiveO2 User Group
- Video Setup Guide
- Support Portal & Instruction Manual
What's in the Box
We designed the Adaptive Contrast system with feedback from our customers.
Each system includes everything you will need to get started:
- 10 LPM air separator system (Upgrade to 20 LPM available)
- 1 AC reservoir
- 1 Basic mask Kit (add more mask kits from the store)
- 1 Choice of hanging option (upgradable to frame kit)
- 1 Basic pulse oximeter
- All silicone tubing
Optional Upgrades:
Concentrator Capacities
You have the option to choose one of two concentrator capacities.
- 10LPM Capacity - Best for single home use (takes 60 min to fill before use).
- 20LPM Capacity - Best for small clinics or athletes looking for a higher-capacity home use system (takes 25 min to fill before use).
- Need more than 20LPM? Check out our dual AC system for professional use.
Specs
- Reservoir: 7’ ft. high x 5’ ft. wide
- Frame: 8’ ft. high x 6’ ft. wide
- Air Separator: 30” inches high x 15” inches wide x 17” inches deep (*leave an 8” border around so it pulls air properly)
- Approximate total space required (without bike): you’ll need a space roughly 10’ high x 7’ wide x 1’ deep
Power Supply
We offer power supply configurations for anywhere in the world. If you are in North America you are using 120V / 60 Hz. If you are outside the United States and do not know your residential voltage please refer to this list.
Financing
We offer affordable equipment financing for organizations and individuals. You can learn more the options available or by calling us.
Shipping FAQ
How much does shipping cost?
Fixed Shipping cost on this two part system is $100 within the continental United States, Alaska and Hawaii additional shipping cost. Canada ship cost $175. The cost of each order is different depending on the size of your shipment, the number of boxes, and your location.
Do you ship internationally?
WHN ships worldwide! We use DHL as our international carrier, as they have proven to be consistently reliable as an international shipping partner. Please note: International orders will not be shipped without a valid email address and phone number. Read more...
How fast is shipping?
Orders most often leave the warehouse within 24 hours of being placed, though in some cases it may take up to 72 hours for an order to ship. Read More...
7 Reviews
-
AC system
Everything as advertised. Oxygen helps.
-
easy set up
works great, i like a lot
-
Amazing!
Highly recommend. This product has changed my life. I have suffered from many traumatic brain injuries and had doctors tell me there was nothing I could do to ease my symptoms. That is until I tried the LiveO2 machines. My brain is so much more clear, I sleep so much better, and my entire life has improved. Thank you, thank you, thank you!
-
Great Results
I'm so glad I made this investment. My health is already changing in as little as three weeks. I've had more energy. Better focus. Reduced inflammation. A change in appetite. I bought this product to help with my issues with MS. So far it seems to be working. As a bonus I've also lost weight. Feeling good! I can't wait to see how much more improvement I experience over the coming weeks.
-
LIVEO2 ADAPTIVE CONTRAST SYSTEM
We've seen surprising polsitive results from using the system. However the bag seems to have a leak between the -O2 and the +O2 connection. Hope to get it remedied.
-
O2 adaptive contrast
Very effective. Easy to use and effective.
-
Just As Advertised
Everything came as advertised on the website and is almost exactly machine I used at my Chiro office. Love the convenience from home. Do wish it was just a little smaller but I feel it's positively impacting my health. Thanks










